EHR
We developed and validated an accurate in-hospital mortality prediction score in a live EHR for automatic and continuous calculation using a novel model that improved upon SOFA.
The COVID-19 pandemic created an emergent need for a novel, accurate, and location and context-sensitive EHR-computable tool to predict mortality in hospitalized patients with and without COVID-19. Because developing a new score can take years, a predictive model must rely on well-validated scores.
In contrast, COVID-19 is a novel disease for which existing scores may be of limited but unknown predictive value.
As such, a predictive framework relying on multiple previously validated scores that can incorporate new information but only keeps the new inputs that explicitly improve performance is required. Stacked generalization provides a solution. A stacked model is built upon one or more baseline model(s) (e.g. SOFA) and incorporates additional models only when they improve prediction.
Materials and Methods
We developed, verified, and deployed a stacked generalization model to predict mortality using data available in the EHR by combining five previously validated scores and additional novel variables reported to be associated with COVID-19-specific mortality.
We verified the model with prospectively collected data from 12 hospitals in Colorado between March 2020 and July 2020. We compared the area under the receiver operator curve (AUROC) for the new model to the SOFA score and the Charlson Comorbidity Index.
Results
The prospective cohort included 27,296 encounters, of which 1,358 (5.0%) were positive for SARS-CoV-2, 4,494 (16.5%) required intensive care unit care, 1,480 (5.4%) required mechanical ventilation, and 717 (2.6%) ended in death. The Charlson Comorbidity Index and SOFA scores predicted mortality with an AUROC of 0.72 and 0.90, respectively. Our novel score predicted mortality with AUROC 0.94. In the subset of patients with COVID-19, the stacked model predicted mortality with AUROC 0.90, whereas SOFA had AUROC of 0.85.
Discussion
Stacked regression allows a flexible, updatable, live-implementable, ethically defensible predictive analytics tool for decision support that begins with validated models and includes only novel information that improves prediction.
read the paper abstract at https://academic.oup.com/jamia/advance-article/doi/10.1093/jamia/ocab100/6273353
read the entire paper at https://academic.oup.com/jamia/advance-article-pdf/doi/10.1093/jamia/ocab100/37905236/ocab100.pdf
Lire l'article complet sur : academic.oup.com

Patient travel history can be crucial in evaluating evolving infectious disease events. Such information can be challenging to acquire in electronic health records, as it is often available only in unstructured text.
Objective: This study aims to assess the feasibility of annotating and automatically extracting travel history mentions from unstructured clinical documents in the Department of Veterans Affairs across disparate health care facilities and among millions of patients. Information about travel exposure augments existing surveillance applications for increased preparedness in responding quickly to public health threats.
Methods: Clinical documents related to arboviral disease were annotated following selection using a semiautomated bootstrapping process. Using annotated instances as training data, models were developed to extract from unstructured clinical text any mention of affirmed travel locations outside of the continental United States. Automated text processing models were evaluated, involving machine learning and neural language models for extraction accuracy.
Results: Among 4584 annotated instances, 2659 (58%) contained an affirmed mention of travel history, while 347 (7.6%) were negated. Interannotator agreement resulted in a document-level Cohen kappa of 0.776. Automated text processing accuracy (F1 85.6, 95% CI 82.5-87.9) and computational burden were acceptable such that the system can provide a rapid screen for public health events.
Conclusions: Automated extraction of patient travel history from clinical documents is feasible for enhanced passive surveillance public health systems.
Without such a system, it would usually be necessary to manually review charts to identify recent travel or lack of travel, use an electronic health record that enforces travel history documentation, or ignore this potential source of information altogether.
The development of this tool was initially motivated by emergent arboviral diseases. More recently, this system was used in the early phases of response to COVID-19 in the United States, although its utility was limited to a relatively brief window due to the rapid domestic spread of the virus.
Such systems may aid future efforts to prevent and contain the spread of infectious diseases.
read the study at https://publichealth.jmir.org/2021/3/e26719
Lire l'article complet sur : publichealth.jmir.org

While Electronic Health Record (EHR) has witnessed a huge boom in the wake of the COVID-19 pandemic, it has paved the path for the proliferation of telehealth facilities, through advanced data analytics and EHR dashboards.
It goes without saying that the outbreak of this life-threatening pandemic has exerted significant influence on population health and wellbeing. As healthcare organizations are building up efforts to treat COVID-19 patients, their IT health marketers are looking to equip them with tools to manage cases, analyze data and assess patients remotely.
Use of digital technology in our everyday life – smartphones, tablets and web enabled devices, has already radically transformed our world. A more considerable and ideal flow of information within a digital health care framework, created by Electronic Health Records (EHRs), encloses and supports digital progress and can transform the delivery of healthcare, as the information is readily available whenever and wherever needed.
One of the leading aspects of EHRs is that the health information can be generated and controlled by authorized providers in a digital format. Such data has the potential of being shared with other providers and healthcare organization such as labs, consultants, medical imaging facilities, pharmacies and clinics – carrying information from all clinicians involved in patient’s care. This does not only provide coordinated and efficient patient care but also increases patient participation, improve diagnostics and patient outcomes by reducing medical errors.
It also plays a leading role in enhancing privacy and security of patient data while serving as a cost-saving mechanism owing to reduced paperwork.
Here are 3 ways medical providers are using Electronic Health Records (EHRs) to treat COVID-19 patients:
Accelerating Use of Telehealth
In the course of this pandemic, implementation of telehealth services has skyrocketed, primarily owing to over-crowing at hospitals and the intense need for social distancing. What initially began as an endeavor to curb the spread of the virus has now become a leading technological tool facilitating healthcare across the globe.
Hence, amongst the widely accredited benefits of telehealth is the tendency to slow down the spread of the disease by keeping the people at risk out of waiting areas, maintaining social distancing and reducing their contact with healthcare personnel. It also permits patients who are not suffering from COVID-19 to continue to receive their care while staying at home. Moreover, the service has proven more useful for older people who are at higher risk during the spread of this disease.
From the provider’s perspective, telehealth increases the capacity of the providers’ staff, facilitating the treatment of a greater number of patients at one time while protecting clinicians and health professionals by reducing physical contact with the infected patients. Suspected cases or patients with mild symptoms that do not require hospital care can be monitored remotely, making the beds readily available for serious complicated cases. According to a recent survey, it has been found that telehealth has a higher satisfaction rate than other healthcare options.
Advanced Data Analytics
Data analysis is the science of analyzing raw data in order to interpret all the information. These data analytics methods can reveal valuable trends and metrics and then this information can be used to optimize procedures to enhance the overall efficiency of the healthcare facility. With the implementation of these data analytics, heath care providers can anticipate what is coming, the needs, filtering and identifying COVID-19 patients and managing the health of population in a more organized way by remaining well prepared ahead of time.
Advanced data analytics have also predominantly enhanced data access, which is of utmost concern to all providers. This is particularly of significant use in the current pandemic situation, where remote patient monitoring is the need of the hour.
At the same time, data analytics help boost interoperability, making it easy to stay updated about critical features as well as rapid demands of the pandemic. Also, since data analytics offer an analysis of telehealth visit volumes and durations, it aids the providers in gauging the demand for telemedicine solution providers across facilities and across health systems.
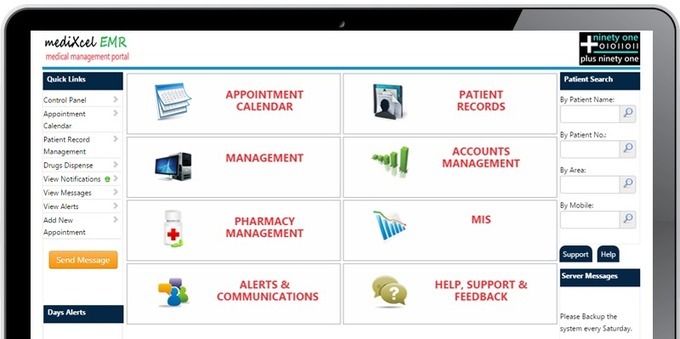
Implementing EHR Dashboard
In order to track COVID-19 patients, use of EHR Dashboard allows clinicians to quickly pinpoint changes in the patient’s conditions that require intervention.
This greatly assists providers to run the practice more efficiently as all the information is readily available at one place. Once logged into the EHR Dashboard, providers can go through a list of patients coming in for that particular day (including who has already checked in and is ready to be examined) along with an easy approach to the cause for the visit and clinical history.
A favorable dashboard provides a rapid glance into essential information, also permits users to generate reports or assess the data operating the analytics effortlessly – all within a few clicks.
Providers have put EHR dashboards to good use as a key component of critical decision making at crucial times such as the current COVID-19 crisis. Recognizing the fact that data interoperability remains the key to maintaining patient care, EHR dashboards allow collaboration amongst healthcare organizations and providers to allow easy access to the state’s most functional health systems and labs.
They, thereby, play a crucial role in promoting health data exchange and in making predictions about the spread of the coronavirus using trends and patterns.
However, there are still limits to the use of this innovative and life-saving digital technology. There are limitations to who can access virtual medicine (from the patients’ perspective), owing to the digital divide or economic hardship. For many people, nevertheless, electronic health tools are a major way to fight back against COVID-19.
Lire l'article complet sur : blog.curemd.com




